With COVID-19 vaccine rollouts ramping up globally and infection cases going down, there’s finally hope of life returning to “normal”. But what does it mean for a pandemic to “end”? Is that even possible? We examine some common outcomes for pandemics to understand how this pandemic could wrap up.
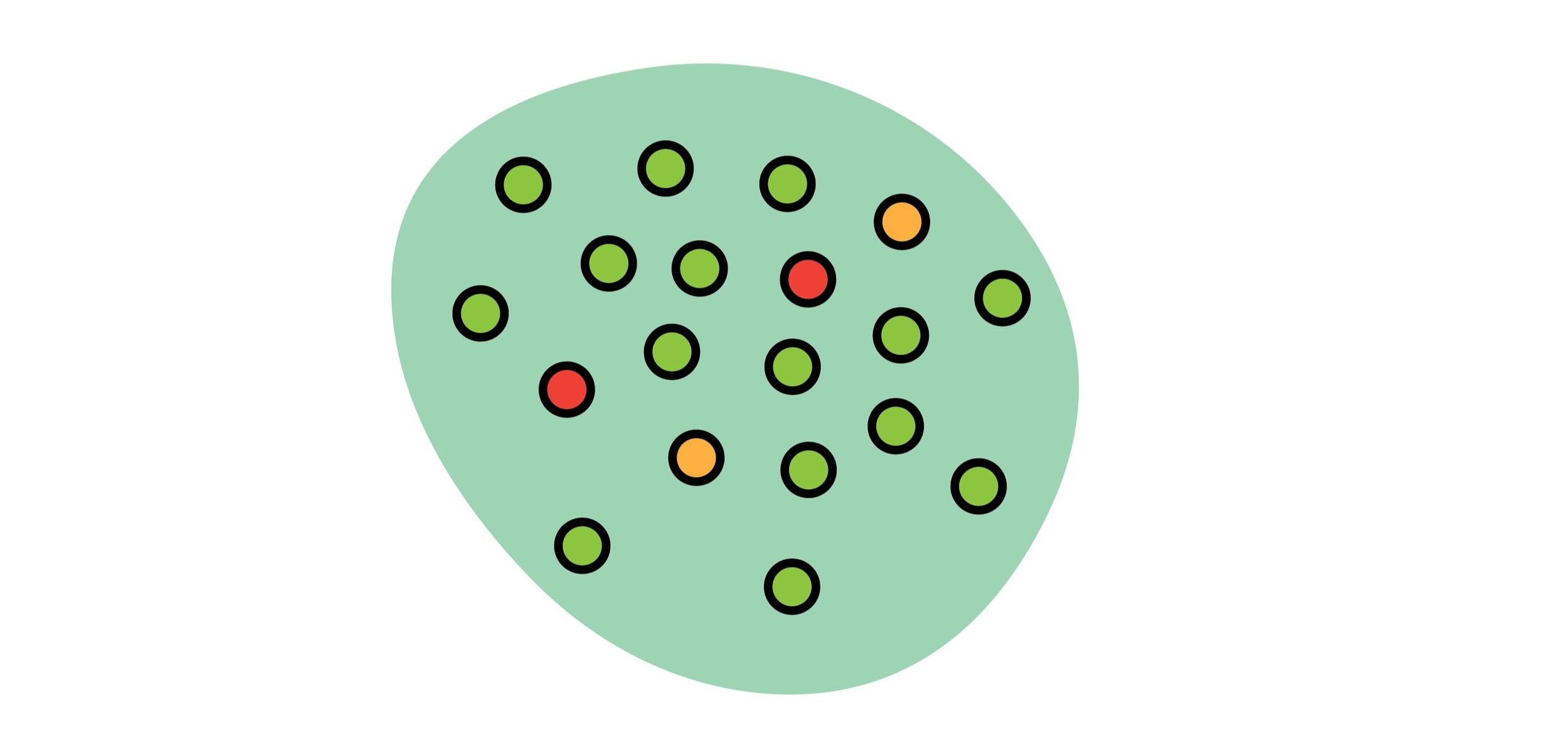
HERD IMMUNITY
The idea of ‘Herd Immunity’ has been talked about frequently in the last year but, what is it and how do we achieve it?
If enough people develop immunity to a certain disease, they are able to contain the spread of the pathogen to other people. We are able to develop immunity through exposure to the pathogen, either by vaccination or infection.
The percentage of people who need to be immune to the disease to establish herd immunity is highly dependent on how transmissible the pathogen is. For example, measles is the most transmissible pathogen we know and in a completely vulnerable population creates up to 15 infections per 1 person infected. Herd immunity is established when 95% of a population is immune. With COVID, experts are still trying to determine what that number is. As more transmissible variants have circulated throughout the world, the general consensus is that between 70% and 85% of the population needs immunity to establish herd immunity.
EFFECTIVE TREATMENTS
At the beginning of the pandemic, there was a race to find remedies for severe infections. From March to June of 2020, around 6% of infections in the United States were resulting in deaths. Doctors were focused on symptom management interventions like ventilation because it was unknown which available drugs would be effective. Hydroxychloroquine and interferon quickly became candidates but were found to be ineffective.
Towards the end of the year, before any vaccines were approved, around 2% of infections were resulting in death. The FDA approved a two drug combination for severe cases that consisted of antiviral medication and an autoimmune drug that helps direct antibody responses.
Vaccines are known as a type of treatment called prophylaxis, meaning that it is a drug taken before exposure to prevent infection. Another type of prophylaxis is used to prevent HIV infections. It essentially works by inhibiting the replication of HIV if somebody is exposed to it and can contribute to herd immunity. This type of drug must be continually ingested to keep immunity because it is quickly metabolized by the body. Drugs like these are in the works for COVID and can be especially useful for people who cannot take vaccines due to allergies.
MUTATIONS
We’ve heard a lot about mutations and variants that have made certain strains of COVID-19 more transmissible and potentially resistant to the vaccines in the field. However, it is possible that mutations can lead to the end of a pandemic. If we look back to the Spanish Flu in the early 1900s, we saw that the dominant strain eventually became a more transmissible variant but less deadly. It became more like the seasonal flu rather than a death sentence.
Coronaviruses can cause a bevy of respiratory infections in humans and are actually one of the pathogens responsible for the common cold. It’s an unlikely candidate for the end of this pandemic but still possible.
NON-PHARMACEUTICAL INTERVENTIONS
This is a fancy word for what we’ve been told since the beginning of the pandemic. Social distancing, wearing masks, and keeping your hands clean can help slow the spread of disease. Even with some infections if enough people kept their distance and prevented the spread the pathogen would eventually fade. We’ve seen this in a few countries like South Korea, Taiwan, and New Zealand where sweeping measures were taken across the country including mask mandates, lockdowns, and robust testing programs.
NO END
Only two pathogens have truly been eradicated, Smallpox and Rinderpest. Both of these viruses were only able to infect and spread through one organism each, humans and cows. Pathogens that have “natural reservoirs” or undomesticated animal hosts are unlikely to ever truly be eradicated. The bacteria that caused the black plague is still around in fleas and causes up to 10 reported infections per year but now that we have effective antibiotics, it’s chances to become a pandemic are slim to none.
Currently, there is massive investment by governments and health organizations to eradicate a number of diseases like polio, malaria and guinea worm.
Polio is another example of a highly infectious disease that requires a high degree of herd immunity. It is currently eradicated in most of the developed world but there are still a few hundred reported cases per year.
Malaria has been the subject of public health initiatives since the colonization of Africa. While a cure exists, as long as one mosquito still carries the parasite then it will never be eradicated. There has actually been extensive research looking into how consequential a forced mosquito extinction would be due to how many diseases mosquitoes spread to humans every year.
The COVID-19 pandemic will end but there is still work to be done. Get a vaccine if you’re able to and afterwards still social distance, wear a mask, and wash your hands.
Writing by Ryan Mathura, Public Health Innovation Analyst
Ryan is a Master of Public Health Student at Emory University studying Health Policy and Management. He has a background in immunology and worked in vaccine R&D before attending Emory.
Graphics by Sophie Becker, Design Strategist
Sophie is a design strategist at Orange Sparkle Ball. She is a recent graduate from RIT and holds a bachelor’s in industrial design and psychology. Her studies informed her interest in using design thinking to communicate abstract and complex ideas, particularly in public health.